Metabolic Syndrome Overview
- Metabolic syndrome (MS) refers to a collection of 5 risk factors that increases the risk for diabetes (type 2) and heart disease. These factors are abdominal obesity (belly fat), elevated blood pressure, elevated blood sugar, low HDL (“good”) cholesterol, and high triglycerides (another type of blood fat).1
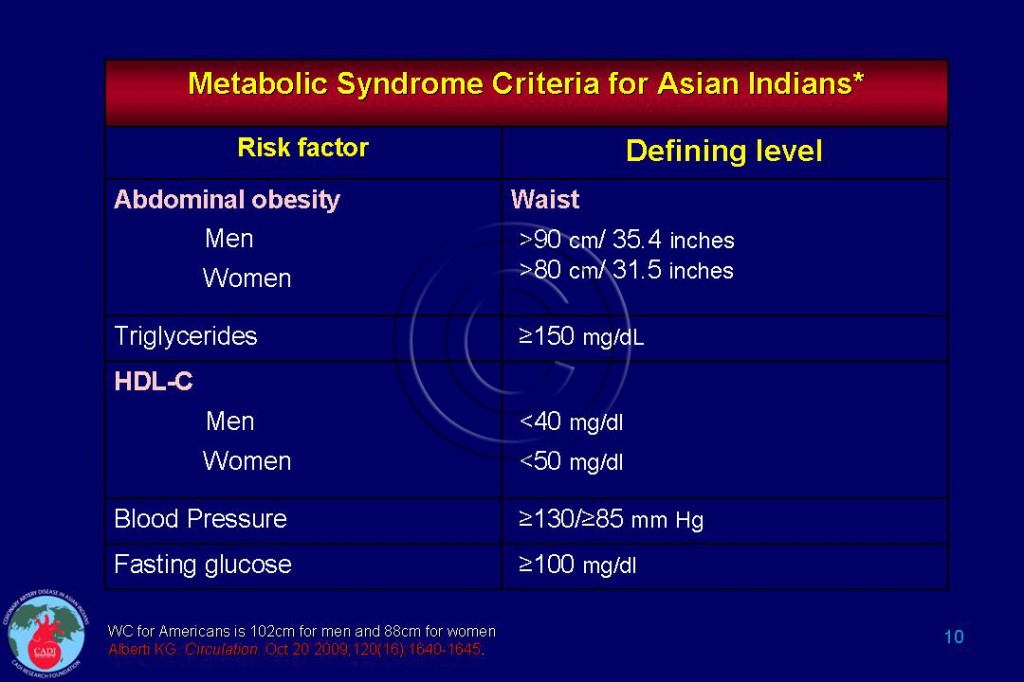
- However, the blood pressure and glucose levels used to define MS are lower than guideline- recommended threshold for pharmacological treatment for these risk factors Table 010.2 There are no thresholds for pharmacological treatment aimed at raising HDL cholesterol and lowering triglycerides. Identification of MS may help physicians to recognize patients at increased risk who may not be recognized as such by current guidelines.3
- People with metabolic syndrome have a 5-fold risk of diabetes and 2-fold risk of developing cardiovascular disease (CVD) compared to people without this condition, with a tendency for greater risk in women.1, 4-6
- The long-term risk is even higher with 30-40% of people with metabolic syndrome developing a heart attack, stroke, or diabetes in the following 20 years.7 Despite their increased cardiovascular risk, most patients with MS remain undiagnosed and untreated.8
- In patients with the metabolic syndrome, but without diabetes, the risk is intermediate between non-diabetics and diabetics.5 6 However, the risk imparted by MS maybe higher than that of diabetes because the prevalence of MS is 40% in the US compared to 10% for diabetes.9
- MS also confers a heighted risk of death from heart disease─ 2 fold higher in men and 3-fold higher in women. The overall death rate (death from all causes) was 44% higher in men and 38% higher in women with MS6 (see MetS and CVD). This suggests that the risk from metabolic syndrome is not limited to diabetes or heart disease.
- Low intakes of fiber and higher consumption of sugar-sweetened beverages and high glycemic load are major contributors to MS as well as diabetes.10-12
- Controlling dyslipidemia requires strategies appropriate to a patient’s individual characteristics and the underlying lipid disorder.
- Higher medical care costs have been associated with each of the MS components present except prediabetes. After full adjustment, hypertension ($550), obesity ($366), low HDL ($363), and high triglycerides ($317) were significantly associated with higher annual costs. Development of diabetes or hospitalization for CVD accounted for the excess cost.13
- The average annual total costs of subjects with metabolic syndrome in the US are 60% higher than those without MS ($5,732 vs. $3,581), and 30% higher for those who also have diabetes ( $7,896 vs. $6,038).14
- MS develops at a younger age, lower BMI, and lower waist circumference among Asian Indians than whites (See MetS in Asian Indians).15
- Recently, several major organizations have proposed a unified definition for the metabolic syndrome, with specific lower cut-off points for waist circumference in Asians (See MetS Criteria).16
- MS patients not meeting established treatment criteria for lipids, glucose or blood pressure should trigger intensive lifestyle counseling focused on physical activity, diet and weight loss.3 Aggressive lifestyle modifications such as regular physical activity, weight loss, and reduced glycemic load can prevent or delay the development of diabetes, heart disease and stroke in people with MS.
Sources
1. Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an american heart association/national heart, lung, and blood institute scientific statement: executive summary. Circulation. Oct 25 2005;112(17):e285-290.
2. Alberti KG, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and international association for the Study of Obesity. Circulation. Oct 20 2009;120(16):1640-1645.
3. Maron D.J, Boden WE, Spertus JA, et al. Impact of Metabolic Syndrome and Diabetes on Prognosis and Outcomes With Early Percutaneous Coronary Intervention in the COURAGE (Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation) Trial. J Am Coll Cardiol. Jul 5 2011;58(2):131-137.
4. Mente A, Yusuf S, Islam S, et al. Metabolic syndrome and risk of acute myocardial infarction a case-control study of 26,903 subjects from 52 countries. J Am Coll Cardiol. May 25 2010;55(21):2390-2398.
5. Mottillo S, Filion KB, Genest J, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. Sep 28 2010;56(14):1113-1132.
6. Hu G, Qiao Q, Tuomilehto J, Balkau B, Borch-Johnsen K, Pyorala K. Prevalence of the metabolic syndrome and its relation to all-cause and cardiovascular mortality in nondiabetic European men and women. Arch Intern Med. May 24 2004;164(10):1066-1076.
7. Wannamethee SG, Shaper AG, Lennon L, Morris RW. Metabolic syndrome vs Framingham Risk Score for prediction of coronary heart disease, stroke, and type 2 diabetes mellitus. Arch Intern Med. Dec 12-26 2005;165(22):2644-2650.
8. Jukema JW, Chiang CW, Ferrieres J, et al. Lipid goals among patients with diabetes or metabolic syndrome: Lipid Treatment Assessment Project (L-TAP) 2. Curr Med Res Opin. Nov 2010;26(11):2589-2597.
9. Cheung BM, Ong KL, Man YB, Wong LY, Lau CP, Lam KS. Prevalence of the metabolic syndrome in the United States National Health and Nutrition Examination Survey 1999-2002 according to different defining criteria. J Clin Hypertens (Greenwich). Aug 2006;8(8):562-570.
10. Sahyoun NR, Jacques PF, Zhang XL, Juan W, McKeown NM. Whole-grain intake is inversely associated with the metabolic syndrome and mortality in older adults. Am J Clin Nutr. Jan 2006;83(1):124-131.
11. McKeown NM, Meigs JB, Liu S, Wilson PW, Jacques PF. Whole-grain intake is favorably associated with metabolic risk factors for type 2 diabetes and cardiovascular disease in the Framingham Offspring Study. Am J Clin Nutr. Aug 2002;76(2):390-398.
12. McKeown NM, Meigs JB, Liu S, Saltzman E, Wilson PW, Jacques PF. Carbohydrate nutrition, insulin resistance, and the prevalence of the metabolic syndrome in the Framingham Offspring Cohort. Diabetes Care. Feb 2004;27(2):538-546.
13. Nichols GA, Moler EJ. Metabolic syndrome components are associated with future medical costs independent of cardiovascular hospitalization and incident diabetes. Metab Syndr Relat Disord. Apr 2011;9(2):127-133.
14. Enas EA, Mohan V, Deepa M, Farooq S, Pazhoor S, Chennikkara H. The metabolic syndrome and dyslipidemia among Asian Indians: a population with high rates of diabetes and premature coronary artery disease. Journal of the cardiometabolic syndrome. Fall 2007;2(4):267-275.
15. Misra A, Misra R, Wijesuriya M, Banerjee D. The metabolic syndrome in South Asians: continuing escalation & possible solutions. Indian J Med Res. Mar 2007;125(3):345-354.
16. Okamura T, Kokubo Y, Watanabe M, et al. A revised definition of the metabolic syndrome predicts coronary artery disease and ischemic stroke after adjusting for low density lipoprotein cholesterol in a 13-year cohort study of Japanese: The Suita Study. Atherosclerosis. Mar 15 2011.