Primary Prevention
- This approach also called high-risk approach aims at identifying individuals with markedly elevated risk factors, but have not suffered a heart attack, and targeting them for interventions. Individuals so identified to be at high risk should be targeted for maximum lifestyle changes as early as two years of age.1
- The high risk approach depends directly on the practicing physicians and other health care workers. Important modifications include adopting a daily exercise regimen, avoiding cigarette smoking and watching not only the weight and saturated fat cholesterol level, but also the waist size and caloric intake. Drug therapy is used when lifestyle measures fail to produce optimum results.2
- The proportion of high-risk cases in a population is directly dependent on the average level and distribution of risk factors. In other words, the mean blood pressure of the population accurately predicts the number of hypertensive individuals and the mean BMI predicts the number of overweight and obese individuals.
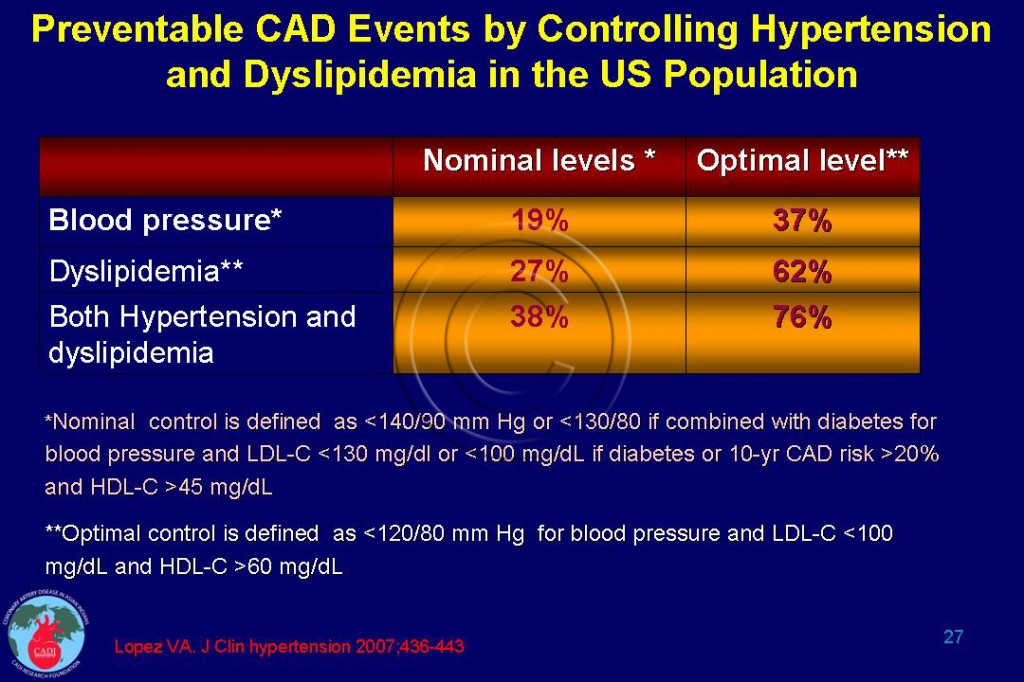
- Several countries like US, Canada, Argentina, Finland, the UK, and Ireland have reported more than 60% decline in CAD death rates in the past 30 years. Approximately, 60-75% of this decline is due to the reduction in the incidence of heart attack from improvements in risk factors (primary prevention). Only about 25% of the decline in CAD death rates is attributed to improvements in case fatality and secondary prevention. The impact of aggressively controlling blood pressure and lipids is given in Table 027.
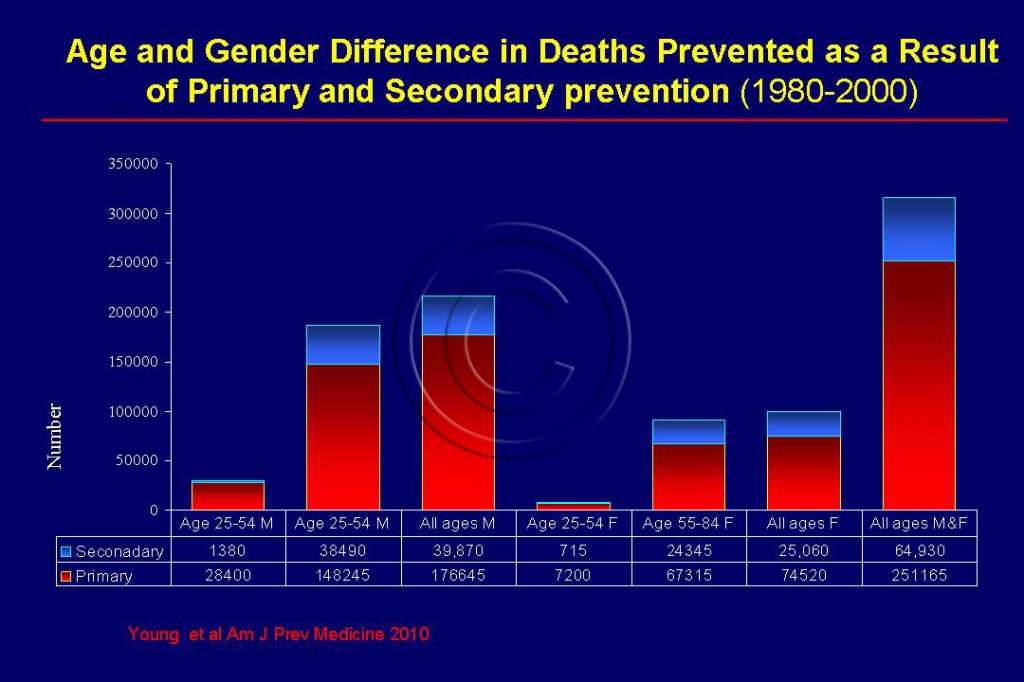
- A recent study reported that the CAD mortality declined 40% from 1980 to 2000 of which approximately half the decline was attributed to favorable changes in CVD risk factors leading to reduced incidence of heart attack and the other half due to advances in treatment of people who survived a heart attack.
- The number of subjects in whom, the intervention is needed to prevent one CVD event will vary in different populations or population subgroups (e.g. women) depending on their underlying prevalence and distribution of risk factors and the incidence rates of disease.
- Clinical trial evidence has shown convincingly that pharmacological treatment of risk factors can prevent events. Innovations have recently been proposed including strategies for dietary sodium reduction and tobacco control, which could prevent more than 1 million deaths per year in low and middle income countries (LMIC) at a cost of approximately US$0.50 per person per year.
- The use of aspirin and low-cost, off-patent drugs for high blood pressure and high lipid levels among patients at high absolute risk of cardiovascular diseases (CVD), which could lead to 2 million fewer deaths per year at a cost of approximately $1.00 per person per year.3, 4
- Family history of premature heart disease should be considered in identifying high risk individuals who have double the risk of heart disease compared to those without such a history at any given level of traditional risk factors.
- Treatment and risk reduction should be more aggressive, with risk scores modified for ethnicity, or ethnic specific tables used. Lower body mass index (BMI) and waist circumference (WC) should be used in identifying abdominal obesity, and metabolic syndrome among Asian Indians.5, 6
- Use of safe and inexpensive pharmacologic therapies in fixed-dose combination, such as the polypill, is another promising avenue for the prevention of CVD.7
- The millions of individuals with risk factors and disease require adaptation of healthcare delivery systems, strengthening of primary care, training and deployment of local health practitioners, development of referral and information systems, production of practice guidelines adapted to the realities of the countries, development of simple diagnostic tools, and implementation of low-cost pharmacologic and nonpharmacologic treatments, and evaluation and monitoring systems.8
- Only the primary prevention and primordial prevention have the potential of preventing a first heart attack or stroke. Primary prevention has been consistently shown to outweigh secondary prevention. However, governments and healthcare personnel give more attention to the latter. See Figure 105.
- Although both physicians and patients are generally well motivated to act in high-risk patients, the success in modification of the lifestyle is generally low, if the remainder of the population continues to indulge in unhealthy habits (see Primordial Prevention).
Sources
1. McCrindle BW, Urbina EM, Dennison BA, et al. Drug therapy of high-risk lipid abnormalities in children and adolescents: a scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee, Council of Cardiovascular Disease in the Young, with the Council on Cardiovascular Nursing. Circulation. Apr 10 2007;115(14):1948-1967.
2. Enas EA. How to Beat the Heart Disease Epidemic among South Asians: A Prevention and Management Guide for Asian Indians and their Doctors. Downers Grove: Advanced Heart Lipid Clinic USA; 2011.
3. Asaria P, Chisholm D, Mathers C, Ezzati M, Beaglehole R. Chronic disease prevention: health effects and financial costs of strategies to reduce salt intake and control tobacco use. Lancet. Dec 15 2007;370(9604):2044-2053.
4. Lim SS, Gaziano TA, Gakidou E, et al. Prevention of cardiovascular disease in high-risk individuals in low-income and middle-income countries: health effects and costs. Lancet. Dec 15 2007;370(9604):2054-2062.
5. Enas EA, Singh V, Munjal YP, Bhandari S, Yadave RD, Manchanda SC. Reducing the burden of coronary artery disease in India: challenges and opportunities. Indian Heart J. Mar-Apr 2008;60(2):161-175.
6. Enas EA, Singh V, Gupta R, Patel R, et al. Recommendations of the Second Indo-US Health Summit for the prevention and control of cardiovascular disease among Asian Indians. Indian Heart J. 2009;61:265-74.
7. Lonn E, Bosch J, Teo KK, Pais P, Xavier D, Yusuf S. The polypill in the prevention of cardiovascular diseases: key concepts, current status, challenges, and future directions. Circulation. Nov 16 2010;122(20):2078-2088.
8. Paradis G, Chiolero A. The cardiovascular and chronic diseases epidemic in low- and middle-income countries a global health challenge. J Am Coll Cardiol. Apr 26 2011;57(17):1775-1777.