LDL─The Principal Cause of Heart Disease
- Evidence from controlled clinical trials has corroborated a causal role for LDL-C in atherogenesis. Lowering of LDL-C levels is associated with reduced risk of cardiovascular disease (CVD) mortality and morbidity rates that is directly proportional to the magnitude of LDL-C reduction.1
- Epidemiological and interventional studies show that a 50 mg/dL decrease in LDL-C results in 32% reduction in heart attack and 20% reduction in stroke whereas a 10 mm Hg decrease in systolic blood pressure results in 22% reduction in MACE (major acute coronary events) and 41% reduction in stroke.1
- Studies of individuals with genetically low LDL-C levels (PCSK9 gene loss of function) have shown that a lifelong 1% reduction in LDL-C confers a 3% reduction in CVD ─ far greater than 1% reduction observed in randomized clinical trials that usually lasts only 5 years.1-3
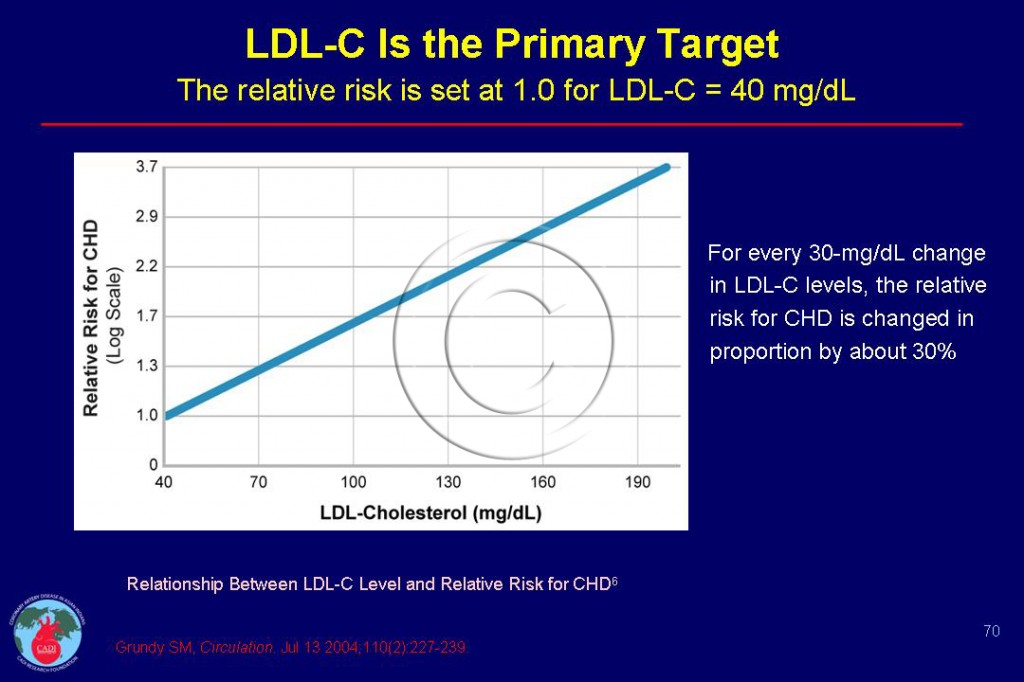
- The optimum LDL-C level is currently standardized at 40 mg/dL.4 Grundy et al4 have demonstrated a log-linear relationship between increased serum LDL-C levels and increased relative risk for CAD. The data plotted in this way suggest that for every 1 mg/dL increase in LDL-C, the relative risk increases by 1%. Thus, an individual with an LDL-C of 70 mg/dL has a 30% higher risk than one with an LDL-C of 40 mg/dL as shown in Figure 070.4
- Intense LDL-C lowering yields superior benefits than moderate lowering; the absolute benefit is related to the person’s’ baseline absolute risk and the degree of LDL-C lowering but not the initial LDL-C level.5
- In the JUPITER Study of adults with LDL-C <130 mg/dl, those who were randomized to rosuvastain had a 45 % reduction in heart attack and other CVD outcomes. Strikingly, those who achieved an LDL-C <50 mg/dl had a 65% reduction in CVD outcome compared to just 24% among those who did not achieve LDL-C <50 mg/dl. Conversely those who had LDL-C >70 mg/dl had no benefit (possibly due to not taking the statin as directed). It is worth noting that most of these subjects were at low-risk of CAD and had low LDL-C of 108 mg/dl).6
- It is worth highlighting that those achieving LDL-C <50 mg/dl had no increase in side effects compared to those who had LDL-C >50 mg/dl. Thus, greater reduction in LDL-C and CVD risk can be achieved without a systematic increase in adverse events (see Statin side effects).6
- The Cholesterol Treatment Trialists’ (CTT) Collaborators have showed that more-intensive therapy produces further reductions in each category of major CVD events (coronary death, heart attack, coronary angioplasty/stent/bypass, and ischemic stroke). The reductions in risk per mmol/L (40 mg/dl) reduction in LDL cholesterol were similar, irrespective of the baseline concentration of LDL cholesterol, even in patients with baseline LDL cholesterol less than 75mg/dl.7
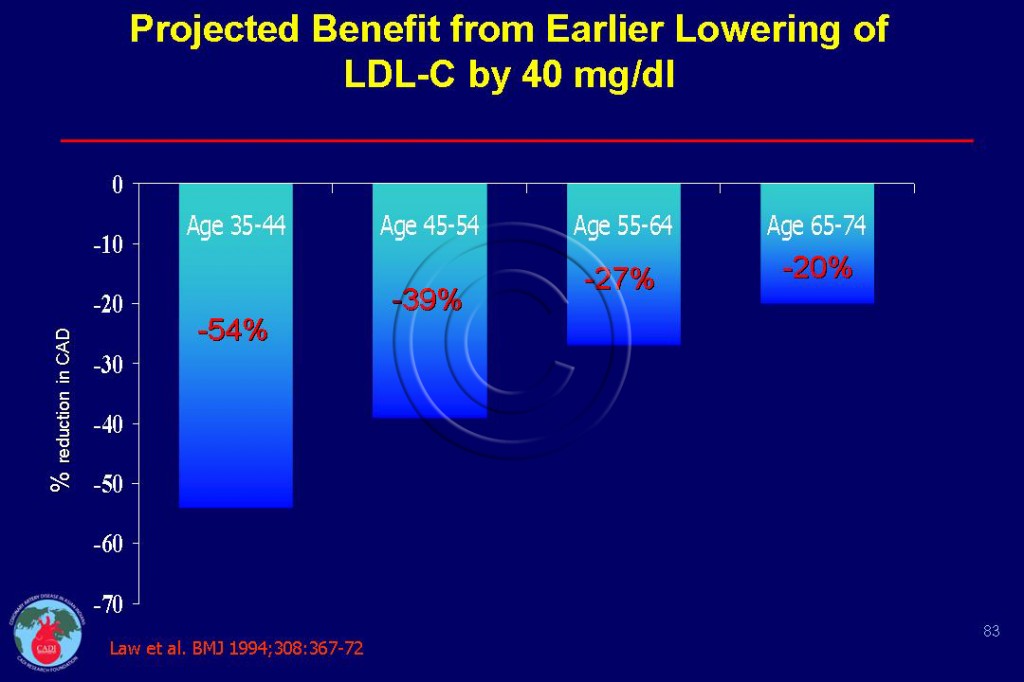
- In sharp contrast, earlier lowering of LDL-C confers greater benefits as shown in Figure 083.8 For instance a 40mg decrease in LDL-c reduce CVD risk by 54% at age 35 compared to only 20% at age 65.
- These results do not imply that an LDL-cholesterol concentration of less than 75mg/dl should be achieved in every low-risk person but the treatment should not be denied in high risk individuals such as those with heart disease, stroke, diabetes and metabolic syndrome.7
- LDL-C lowering reduces CVD risk in women, elderly, people with chronic kidney disease and different levels of CVD risk (Framingham Risk Score). 9-12
- The JUPITER Trial demonstrated that, in primary prevention rosuvastatin reduced CVD events in women with a relative risk reduction similar to that in men, a finding supported by meta-analysis of primary prevention.9
- An 80 mg/dL reduction in LDL-C and/or non-HDL-C confers a 60-80% reduction in CVD after 5 years of treatment (1:1 relationship).1
- Earlier guidelines developed by the U.S. National Cholesterol Education Program (NCEP) Adult Treatment Panel (ATP) have evolved to include LDL-C < 100 mg/dL as the optimal goal for primary prevention in persons with multiple CHD risk factors and LDL-C < 70 mg/dL as an optional goal for very high risk patients.4 The latter is also considered a reasonable target for high risk patients with CVD. Similar guidelines have also been adopted in Europe and Canada.13, 14
- Pharmaco-economic analyses have suggested that higher LDL-C lowering efficacy statins are more cost-effective than lower efficacy statins in terms of LDL-C reduction and goal attainment, quality-adjusted life years (QALY) and projected CVD risk reduction.15, 16 Conversely, switching to a low potency statin results in increased LDL-C levels and lower goal attainment.17
- Although LDL-C goal attainment rates have overall improved during the past decade, only about one-third of high-risk patients with CVD attain levels of LDL-C < 70 mg/dL.17, 18 Given the well-established association between LDL-C lowering and CVD risk reduction, more intensive statin therapy with high potency statins (such as atorvastatin or rosuvastain in high doses) is necessary to achieve the specific targets.1, 17, 19 It is possible that some patients who do not attain LDL-C goals are unwilling to take or intolerant of high dose statin therapy or physicians may be reluctant to use high-dose statins.1
- In a recent analysis of a managed care database in the U.S. (n = 284,915), the proportion of high risk patients with CVD treated with lipid-lowering therapy (LLT) (including statins, niacin, fibrates, bile acid sequestrants, ezetimibe/simvastatin, and ezetimibe,) increased steadily from 59% to 71% from January 2004 to August 2008.7
- Combinations therapy (with niacin, fibrates, ezetemibe or resin) may help to limit the need for higher statin doses in those patients requiring more intensive LDL-C reductions (e.g. > 50%) and provide greater drug adherence as well.18 While the lipid-lowering efficacies of these combination therapies are known, randomized clinical trials assessing the effects of these therapies on CVD outcomes are still awaited.
- Much of the progress in reducing CVD and mortality, is largely attributed to improved cholesterol management, especially the use of higher efficacy LDL-C lowering agents.
- At a given level of cholesterol, Indians have a lower LDL-C (due to high triglycerides that artificially lowers LDL-C). At a given LDL-C level, Indians have higher risk because of high levels of lipoprotein(a), low levels of HDL-C and possibly dysfunctional HDL-C particles ( See Asian Indian Dyslipidemia).
- The recommended lipid goals are 30 mg/dl lower for Indians than that recommended by NCEP for Americans. Accordingly, LDL-C <100 mg/dl and non-HDL-C <130 mg/dl is recommended for most Indians; LDL-C <70 mg/dl and non-HDL-C <100 mg/dl g/dl is recommended for Indians with CAD, diabetes, metabolic syndrome, high lipoprotein(a) or high homocysteine levels.1, 20, 21
- Although statins have become the mainstay of lowering LDL-C, weight reduction of 10 kg can decrease LDL-C by 8mg/dl and dietary modification can reduce LDL-C by 40 mg/dl ( See Functional foods).22 23
Sources
1. Enas E.A., Hancy Chennikkara Pazhoor MD, Arun Kuruvila MBBS, Krishnaswami Vijayaraghavan MD F. Intensive Statin Therapy for Indians:Part I Benefits. Indian Heart J 2011; 63: 211-227.
2. Cohen JC, Boerwinkle E, Mosley TH, Jr., Hobbs HH. Sequence variations in PCSK9, low LDL, and protection against coronary heart disease. N Engl J Med. Mar 23 2006;354(12):1264-1272.
3. Benn M., Nordestgaard BG, Grande P, Schnohr P, Tybjaerg-Hansen A. PCSK9 R46L, low-density lipoprotein cholesterol levels, and risk of ischemic heart disease: 3 independent studies and meta-analyses. J Am Coll Cardiol. Jun 22 2010;55(25):2833-2842.
4. Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. Jul 13 2004;110(2):227-239.
5. Enas E A, Senthilkumar. Coronary Artery Disease In Asian Indians: An Update And Review . The Internet Journal of Cardiology 2001
2011;1:avaible at The Internet Journal of Cardiology accessed Dec 1, 2010.
6. Hsia J, Macfadyen JG, Monyak J, Ridker PM. Cardiovascular Event Reduction and Adverse Events Among Subjects Attaining Low-Density Lipoprotein Cholesterol <50 mg/dl With Rosuvastatin The JUPITER Trial (Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin). J Am Coll Cardiol. Apr 19 2011;57(16):1666-1675.
7. Baigent C, Blackwell L, Emberson J, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. Nov 13 2010;376(9753):1670-1681.
8. Law MR, Wald NJ, Thompson SG. By how much and how quickly does reduction in serum cholesterol concentration lower risk of ischaemic heart disease? BMJ. 1994;308(6925):367-372.
9. Mora S, Glynn RJ, Hsia J, MacFadyen JG, Genest J, Ridker PM. Statins for the primary prevention of cardiovascular events in women with elevated high-sensitivity C-reactive protein or dyslipidemia: results from the Justification for the Use of Statins in Prevention: An Intervention Trial Evaluating Rosuvastatin (JUPITER) and meta-analysis of women from primary prevention trials. Circulation. Mar 9 2010;121(9):1069-1077.
10. Glynn RJ, Koenig W, Nordestgaard BG, Shepherd J, Ridker PM. Rosuvastatin for primary prevention in older persons with elevated C-reactive protein and low to average low-density lipoprotein cholesterol levels: exploratory analysis of a randomized trial. Ann Intern Med. Apr 20 2010;152(8):488-496, W174.
11. Ridker PM, MacFadyen J, Cressman M, Glynn RJ. Efficacy of rosuvastatin among men and women with moderate chronic kidney disease and elevated high-sensitivity C-reactive protein: a secondary analysis from the JUPITER (Justification for the Use of Statins in Prevention-an Intervention Trial Evaluating Rosuvastatin) trial. J Am Coll Cardiol. Mar 23 2010;55(12):1266-1273.
12. Ridker PM, Macfadyen JG, Nordestgaard BG, et al. Rosuvastatin for primary prevention among individuals with elevated high-sensitivity c-reactive protein and 5% to 10% and 10% to 20% 10-year risk. Implications of the Justification for Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin (JUPITER) trial for “intermediate risk”. Circ Cardiovasc Qual Outcomes. Sep 2010;3(5):447-452.
13. Genest J, McPherson R, Frohlich J, et al. 2009 Canadian Cardiovascular Society/Canadian guidelines for the diagnosis and treatment of dyslipidemia and prevention of cardiovascular disease in the adult – 2009 recommendations. Can J Cardiol. Oct 2009;25(10):567-579.
14. Graham I, Atar D, Borch-Johnsen K, Boysen G, Durrington PN. European guidelines on cardiovascular disease prevention in clinical practice: executive summary: Fourth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (Constituted by representatives of nine societies and by invited experts). Eur Heart J. Oct 2007;28(19):2375-2414.
15. Ohsfeldt RL, Gandhi SK, Fox KM, McKenney JM. Statin cost-effectiveness comparisons using real-world effectiveness data: formulary implications. Value Health. Dec 2008;11(7):1061-1069.
16. Straka RJ, Mamdani M, Damen J, et al. Economic impacts attributable to the early clinical benefit of atorvastatin therapy–a US managed care perspective. Curr Med Res Opin. Jul 2007;23(7):1517-1529.
17. Foody JM, Sajjan SG, Hu XH, et al. Loss of early gains in low-density lipoprotein cholesterol goal attainment among high-risk patients. J Clin Lipidol. Mar-Apr 2010;4(2):126-132.
18. Catapano AL. Perspectives on low-density lipoprotein cholesterol goal achievement. Curr Med Res Opin. Feb 2009;25(2):431-447.
19. Cullen MW, Stein JH, Gangnon R, McBride PE, Keevil JG. National improvements in low-density lipoprotein cholesterol management of individuals at high coronary risk: National Health and Nutrition Examination Survey, 1999 to 2002. Am Heart J. Aug 2008;156(2):284-291.
20. Enas EA, Singh V, Munjal YP, et al. Recommendations of the second Indo-U.S. health summit on prevention and control of cardiovascular disease among Asian Indians. Indian Heart J. May-Jun 2009;61(3):265-274.
21. Enas EA, Singh V, Munjal YP, Bhandari S, Yadave RD, Manchanda SC. Reducing the burden of coronary artery disease in India: challenges and opportunities. Indian Heart J. Mar-Apr 2008;60(2):161-175.
22. Catapano AL, Reiner Z, De Backer G, et al. ESC/EAS Guidelines for the management of dyslipidaemias The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Atherosclerosis. Jul 2011;217 Suppl 1:1-44.
23. Jenkins DJ, Jones PJ, Lamarche B, et al. Effect of a dietary portfolio of cholesterol-lowering foods given at 2 levels of intensity of dietary advice on serum lipids in hyperlipidemia: a randomized controlled trial. JAMA. Aug 24 2011;306(8):831-839.