African Americans and Blacks in other Countries
- Several studies have noted higher age-adjusted prevalence, incidence, or mortality rates of cardiovascular disease (CVD) among blacks compared with whites.1-4 Racial differences in CVD prevalence vary by age, with the largest black-white disparities observed in young to middle age.5
- The higher rates of CVD begin in the 30s and 40s (young to middle age).5 More than a quarter of all CVD deaths (28%) among blacks occurred in those aged <65 years, compared with 13% among whites. Reducing these disparities will require a focus on young and middle-aged blacks.5
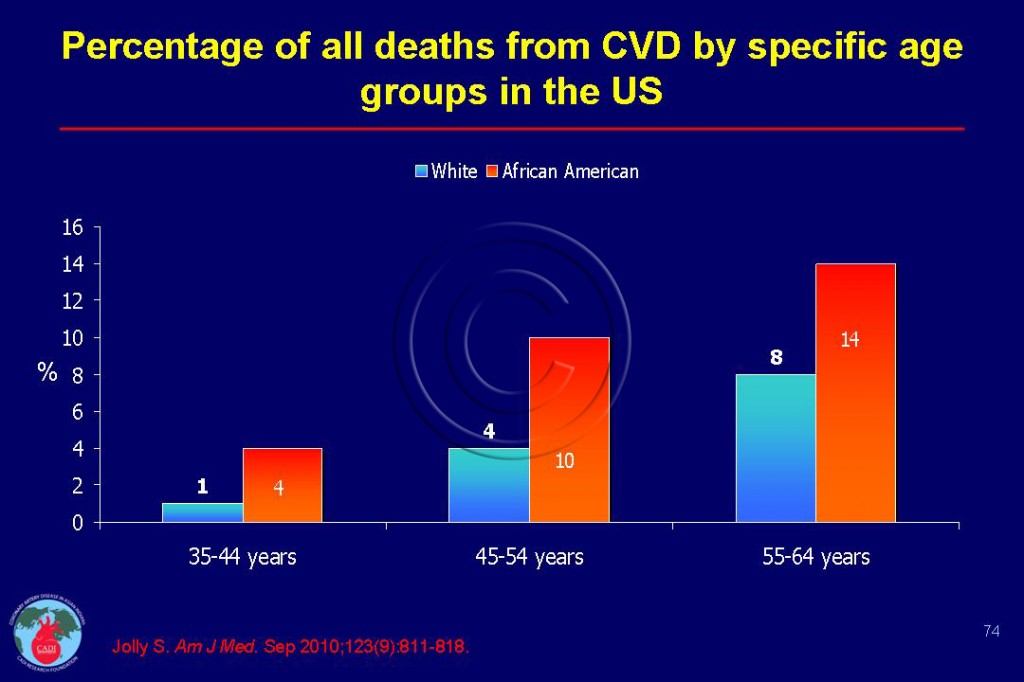
- The percentage of CVD mortality for blacks in US is 4 times that of whites at ages 35-44 (4% vs 1%) and more than double the mortality at ages 45-54 (10% vs 4%) and almost double (16% vs 8%) between ages 55-64 Figure 074.5 The percentage of blacks dying from CVD before age 65 doubles that of whites.5 Blacks had 60% higher prevalence of CVD compared to whites adjusted for risk factors, and access to health care at ages 35-44 decreasing to 20% lower after age 65.5
- The higher burden of CVD among blacks compared to whites occurs at younger ages, possibly due to lower SES (socioeconomic status) and higher prevalence of risk factors.5 Therefore, public health programs should target the prevention and treatment of conditions such as hypertension, diabetes, smoking, and obesity at younger ages in order to reduce the burden of disease in young to middle-aged adults.5
- Younger age groups may be more challenging to reach with these programs, as they are more likely to be uninsured and therefore less likely to have access to medical care, and less likely to be able to afford medications.
- Adherence to medications also may be lower in young and middle-aged adults. These difficulties may be exacerbated by lower awareness among young to middle-aged adults of their CVD risk, and reluctance on the part of clinicians to treat CVD risk factors at younger ages.5
- Although African Americans have higher prevalence of obesity, hypertension and heart failure, they have lower risk of atrial fibrillation.6, 7 After hospitalization for heart failure African-American paradoxically have a 32 % lower short term and 16% lower long-term mortality compared to whites.13
Blacks in other Countries
- More than 20% of the population in rural sub-Saharan Africa has hypertension, and the prevalence of pre-hypertension is more than 40%. Hypertension and high blood pressure were positively linked to: older age, higher BMI, television ownership, less job-related vigorous physical activity, and frequent meat and high-fat food consumption. Frequent intake of fruits and vegetables significantly correlated with lower hypertension prevalence and blood pressure measures. This suggests potential opportunities for prevention measures to improve BMI, dietary intake, and physical activity in this population. 8
- Known CVD risk factors account for approximately 90% of heart attacks observed in African populations, which is consistent with the landmark INTERHEART study. The risk for heart attack increased with higher income and education in the black African group in contrast to findings in the other African groups. A history of hypertension revealed higher risk of heart attack in the black African group than in the other study groups. Contrasting gradients found in socioeconomic class, risk factor patterns, and heart attack risk in the ethnic groups suggest that they are at different stages of the epidemiological transition.9
Differential response to treatment
- In heart attack patients receiving fibrinolysis, moderate or severe bleeding and mortality were significantly higher in African Americans compared with whites, despite the fact that African Americans were 4 years younger. 10 African-American race was an independent correlate of increased bleeding risk.10 Bleeding was associated with increased mortality among both whites and African Americans.10
- Both bleeding and African-American race were associated independently with higher 1-year mortality and African Americans with bleeding had the highest 1-year mortally —even higher than among whites with bleeding.10
- African Americans have enhanced fibrinolytic efficacy and greater systemic fibrinogenolysis after recombinant tissue plasminogen activator (rTPA) compared with whites. This enhanced response to fibrinolysis was associated with increased bleeding risk and need for transfusions in African Americans.11 Decreasing bleeding may represent an opportunity for improving outcomes of these patients.
- Race-related variations in CVD outcomes have been presumed to be related to differences in baseline characteristics, patient management (including the use of medications), diagnostic and therapeutic procedures, socioeconomic factors (including poor access to care, patient preferences, and lifestyle), and physicians’ cultural or racial biases.12 However, the possibility that African Americans and whites have different genotypes and phenotypes with implications not only for the efficacy and effectiveness of drugs, but also with regards to their safety, remains less well appreciated.
- Some studies have shown race to be a factor in differential response to cardiovascular treatments. This data raised an important hypothesis that perhaps drug safety may also differ by race. Currently, clinical trials—the gold standard that drives practice guidelines and contemporary practice—have too few patients of African-American ancestry to elucidate possible differences. This underscores the need to expand the recruiting of blacks and other minorities in clinical trials.
Sources
1. Giles WH, Kittner SJ, Hebel JR, Losonczy KG, Sherwin RW. Determinants of black-white differences in the risk of cerebral infarction. The National Health and Nutrition Examination Survey Epidemiologic Follow-up Study. Arch Intern Med. 1995;155(12):1319-1324.
2. Jones DW, Chambless LE, Folsom AR, et al. Risk factors for coronary heart disease in African Americans: the atherosclerosis risk in communities study, 1987-1997. Arch Intern Med. Dec 9-23 2002;162(22):2565-2571.
3. Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. Mar 15 2005;111(10):1233-1241.
4. Ferdinand K C. Coronary artery disease in minority racial and ethnic groups in the United States. Am J Cardiol. Jan 16 2006;97(2A):12A-19A.
5. Jolly S, Vittinghoff E, Chattopadhyay A, Bibbins-Domingo K. Higher cardiovascular disease prevalence and mortality among younger blacks compared to whites. Am J Med. Sep 2010;123(9):811-818.
6. Marcus G M, Alonso A, Peralta CA, et al. European ancestry as a risk factor for atrial fibrillation in African Americans. Circulation. Nov 16 2010;122(20):2009-2015.
7. Walker AR, Sareli P. Coronary heart disease: outlook for Africa. J R Soc Med. 1997;90(1):23-27.
8. de Ramirez SS, Enquobahrie DA, Nyadzi G, et al. Prevalence and correlates of hypertension: a cross-sectional study among rural populations in sub-Saharan Africa. J Hum Hypertens. Dec 2010;24(12):786-795.
9. Steyn K, Sliwa K, Hawken S, et al. Risk factors associated with myocardial infarction in Africa: the INTERHEART Africa study. Circulation. Dec 6 2005;112(23):3554-3561.
10. Mehta RH, Stebbins A, Lopes RD, et al. Race, Bleeding, and Outcomes in STEMI Patients Treated with Fibrinolytic Therapy. Am J Med. Jan 2011;124(1):48-57.
11. Sane DC, Califf RM, Topol EJ, Stump DC, Mark DB, Greenberg CS. Bleeding during thrombolytic therapy for acute myocardial infarction: mechanisms and management. Ann Intern Med. Dec 15 1989;111(12):1010-1022.
12. Sonel A F, Good CB, Mulgund J, et al. Racial variations in treatment and outcomes of black and white patients with high-risk non-ST-elevation acute coronary syndromes: insights from CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the ACC/AHA Guidelines?). Circulation. Mar 15 2005;111(10):1225-1232.
13. Gordon HS, Nowlin PR, Maynard D, Berbaum ML, Deswal A. Mortality after hospitalization for heart failure in blacks compared to whites. Am J Cardiol. Mar 1 2010;105(5):694-700.