Principles and Classification
- At least 80% of coronary artery disease (CAD), stroke and diabetes and 40% of the cancer could be avoided through healthy diet, regular physical activity and avoidance of tobacco use1. The scientific knowledge to achieve a new global goal for the prevention of chronic diseases─ a 2% yearly reduction in rates of death from chronic disease over and above projected declines during the next 10 years–already exists.1
- Identifying and reducing risk in the high-risk adult population are the hallmarks of preventive practice today. The decision about prevention strategies is no longer a question of science but of resources, feasibility, and readiness in the community and the government.
- An often ignored aspect of prevention is the phased implementation of interventions─ core, expanded and optimum interventions─ on the basis of the availability of resources as well as the political and community support and the configuration of national health systems.1, 2
- We now have the technology, diagnostic tests and medications to help combat the disease. This, in combination, with appropriate lifestyle changes can significantly reduce the risk factors for these dreaded diseases.
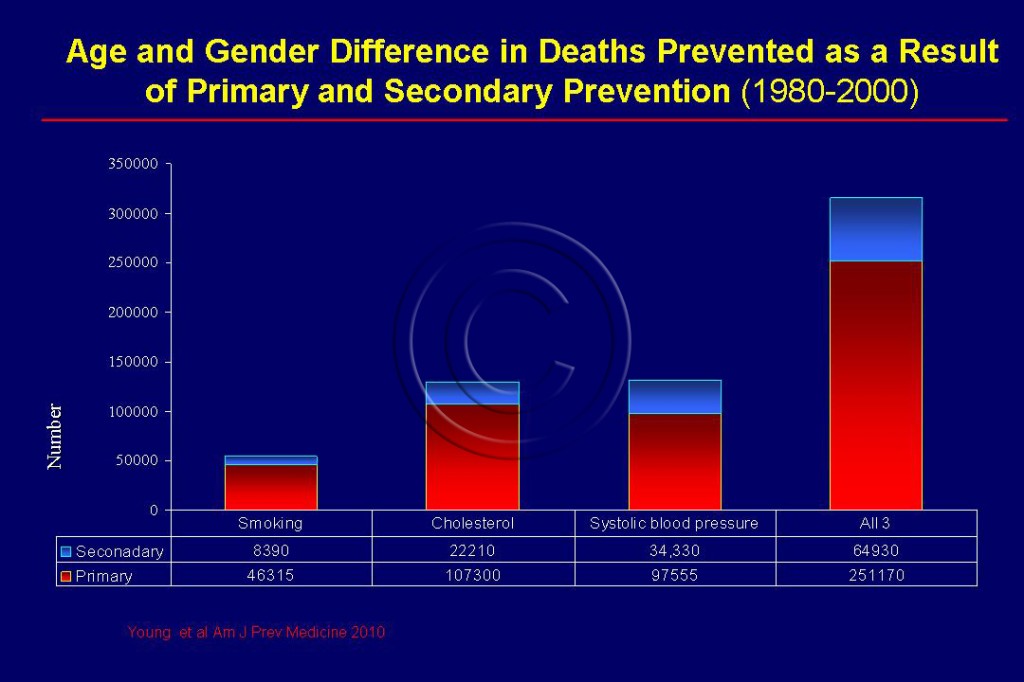
- Early prevention, detection and management of heart disease are vital. The general principle of prevention is to encourage proven lifestyle measures and to prescribe evidence-based effective medications. See Figure 106.
- The growing cardiovascular challenge can be effectively addressed only through preventive public health measures and life style changes according to all experts in the field. The good news is that both heart disease and diabetes have become highly predictable, preventable, and treatable.
- Prevention is the key, particularly in countries such as India where the epidemic is in the process of escalating and there is still time to curtail it.
- The process of atherosclerosis begin in childhood and continue for decades, leading to both nonfatal and fatal cardiovascular events, including heart attacks, stroke, and sudden cardiac death.
- Control of just three major risk factors (high cholesterol, blood pressure, and smoking) accounts for 50-80% of the decline in heart disease observed in many high-income countries.3
Classification of Prevention Strategies
Several cardiovascular disease (CVD) prevention strategies exist as shown. Healthcare providers can implement primary, secondary, and tertiary preventive measures to individual patients whereas involvement of the community and the government is a prerequisite for the implementation and the success of primordial prevention.
- Primordial prevention involves reducing the development and prevalence of CVD risk factors. The prevention may be individual-based or population-based or combined. (see Population Based Prevention and Success)
- Primary prevention involves the avoidance of disease particularly CAD or stroke in high-risk subjects free of disease.
- The purpose of secondary prevention is to avoid recurrence of heart attack in people who have already suffered or who had been diagnosed with heart disease.
- Tertiary prevention usually refers to the use of expensive coronary interventional procedures such as coronary angioplasty, stent, bypass surgery, pacemakers, defibrillators, and left ventricular assist devices (LVAD). The high-tech hospitals that are springing up in low income countries especially India have their resources focused on tertiary prevention.
- We now know that the surge in CAD and their risk factors in varied settings are fuelled by modifiable risk factors which can be reduced by simple strategies. Most of these preventive strategies are in the domain of policy, health system intervention, health promotion and simple quality improvement programs aimed at improving secondary prevention.4 It must also be extended to primary and primordial prevention.
Sources
1. Epping-Jordan JE, Galea G, Tukuitonga C, Beaglehole R. Preventing chronic diseases: taking stepwise action. Lancet. Nov 5 2005;366(9497):1667-1671.
2. Beaglehole R, Ebrahim S, Reddy S, Voute J, Leeder S. Prevention of chronic diseases: a call to action. Lancet. Dec 22 2008;370(9605):2152-2157.
3. Gupta R, Guptha S, Joshi R, Xavier D. Translating evidence into policy for cardiovascular disease control in India. Health Res Policy Syst. 2011;9:8.
4. Prabhakaran D, Yusuf S. Cardiovascular disease in India: lessons learnt & challenges ahead. Indian J Med Res. Nov 2010;132(5):529-530.