Prevention of Heart disease in Asian Indians
- Although cigarette smoking, high blood pressure, high cholesterol, diabetes, obesity, unhealthy diet and sedentary lifestyle do not fully explain the excess coronary artery disease (CAD) in Asian Indians, these time-honored risk factors are clearly associated with CAD in all populations studied and Asian Indians are no exception.1-3 These conventional risk factors are highly correlated with CAD among Indians in India and the diasporas.4, 5
- The prevalence of conventional risk factors in the Indian subcontinent is high and increasing whereas they are low and decreasing among the Indian diasporas. It appears that about 3 in 4 heart attacks in Asian Indians can be attributed to these risk factors. Therefore maximum modification of lifestyle and medications directed at these factors could reduce the CAD risk by about 75%.6 The role of life style modification in the prevention and treatment of CAD among Asian Indians has been recently reviewed.7, 8
- Given the consistent findings of increased prevalence, premature onset and increased mortality from CAD in Asian Indians, there has been much interest in determining the underlying causes in an effort to develop effective prevention and treatment strategies.6
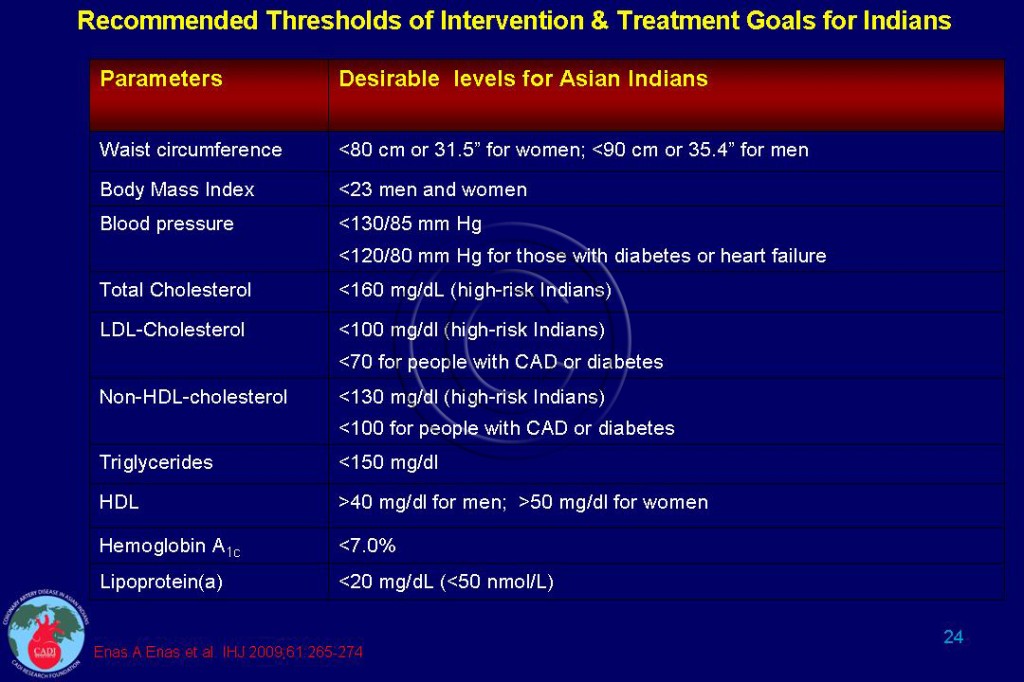
- While mechanistic research to identify the reasons for the younger age of onset of CVD and diabetes and their occurrence at a lower threshold of risk factors is needed, prevention should also begin at a lower threshold and younger age.3, 6 It is worth highlighting that Among Asian Indians, the desirable body mass index (BMI) is <23 in both men and women, and the waist circumference (WC) is <90cm in men and <80cm in women (Table 024).
- Future research and prevention strategies for CAD in South Asians should acknowledge a broad range of risk factors, the heterogeneity of these populations, linguistic and cultural needs, and environmental factors (air pollution).9
Genetic Predisposition
- The most important aspect of prevention of CVD is the early identification of high-risk individuals. Since lipoprotein(a) {Lp(a)} is fully expressed in the first year of life, tracking Lp(a) from childhood may be a better option than focusing on other dyslipidemias which are not expressed until later in life.10
- In a study of Chinese, Malay, and Indian newborns in Singapore, significantly high levels of Lp(a) were found in cord blood of Asian Indians.11 More importantly, the difference in Lp(a) levels in the cord blood paralleled the adult differences in CAD rates in this country.
- In people with elevated Lp(a) levels, the initial preventive and therapeutic goals consist of diligently searching and drastically reducing all concurrent modifiable risk factors with lifestyle modification starting at age 2 and appropriate medication from age 8 onwards.
Prevention of Heart disease in India
- There is an enormous amount of evidence and the required base of science and technology related to CVD prevention, which needs to be translated into concrete action to drastically reduce the burden of heart disease, in India. National level initiatives in non-communicable diseases surveillance, prevention, and control are recent phenomena in India.
- Currently, the translational research seems to be focusing more on the first level (bench to bedside), rather than the second level (bedside to community) in India.12 The possible reasons for this were: inappropriate perception of the problem by policy makers and program managers, lack of global public health guidelines and tools, and inadequate nationally relevant research related to operationalization and cost of public health interventions. 12
- Most intervention studies for the prevention of CVD have been conducted in the West and many of these are not readily applicable to a country like India. In India we need low-cost strategies for screening, which include simple assessment of risk factors by paramedical workers, either by visiting households or through inexpensive health camps.
- India needs a balanced combination of public health and high-risk individualized strategies for the effective control of the CVD epidemic.13 The CAD mortality declined by 40% between 1980 and 2000 in the US; control of the risk factors contributed to a 61% of this decline. Recently, a worksite intervention program in India found a comprehensive, multiple component intervention to have a positive impact on the 10-year Framingham CVD risk score of the workers.14
- In addition, if physicians themselves adopt healthy lifestyles, they are more likely to advise their patients to do so (see Physician Heal Thyself). Therefore, there needs to be intervention trials of different strategies for screening and health promotion. In addition, randomized trials of low-cost approaches to preventing CVD such as the development of the polypill or smoking control would be of importance. In this regard, there should be a national cardiovascular control program, similar to the TB control and malaria eradication programs that the Indian government has supported.
- The WHO recommends a paradigm shift away from the treatment of risk factors in isolation, to a comprehensive CVD management approach. The WHO has also developed CVD risk management packages that use a pragmatic approach with detailed protocol for management of hypertension and advice on life style changes. However, a basic healthcare infrastructure is necessary to apply the CVD risk management package to identify people at high risk, and to ensure appropriate treatment.15
- In order for such a strategy to be successful, four elements are necessary: an enlightened public health policy custom tailored for different parts of the nation, an educated medical profession, an empowered public, and a supportive media.13 The Indian Medical Association, the Indian Medical Council, the Cardiological Society of India, and the Association of Physicians of India should join hand with other medical societies to make reduction in CAD rates in India a lasting reality rather than an elusive dream.
- In 2009, the world mobilized against the threat of pandemic influenza, which killed approximately 15,000 people. Such a mobilization is necessary in India to stem the twin epidemics of heart disease and diabetes which are already killing millions every year. The task is daunting, but we have a moral obligation to support the global fight against CVD and chronic diseases, which are the pandemic of the twenty-first century.16
Sources
1. Forouhi NG, Sattar N, Tillin T, McKeigue PM, Chaturvedi N. Do known risk factors explain the higher coronary heart disease mortality in South Asian compared with European men? Prospective follow-up of the Southall and Brent studies, UK. Diabetologia. Nov 2006;49(11):2580-2588.
2. Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. Sep 11 2004;364(9438):937-952.
3. Enas EA, Singh V, Munjal YP, Bhandari S, Yadave RD, Manchanda SC. Reducing the burden of coronary artery disease in India: challenges and opportunities. Indian Heart J. Mar-Apr 2008;60(2):161-175.
4. Gupta R. Recent trends in coronary heart disease epidemiology in India. Indian Heart J. Mar-Apr 2008;60(2 Suppl B):B4-18.
5. Reddy KS, Prabhakaran D, Chaturvedi V, et al. Methods for establishing a surveillance system for cardiovascular diseases in Indian industrial populations. Bull World Health Organ. Jun 2006;84(6):461-469.
6. Enas EA, Singh V, Gupta R, Patel R, et al. Recommendations of the Second Indo-US Health Summit for the prevention and control of cardiovascular disease among Asian Indians. Indian Heart J. 2009;61:265-74.
7. Enas EA. How to Beat the Heart Disease Epidemic among South Asians: A Prevention and Management Guide for Asian Indians and their Doctors. Downers Grove: Advanced Heart Lipid Clinic USA; 2010.
8. Enas EA. How to Beat the Heart Disease Epidemic among South Asians: A Prevention and Management Guide for Asian Indians and their Doctors. Downers Grove: Advanced Heart Lipid Clinic USA; 2011.
9. Bhopal R, Unwin N, White M, et al. Heterogeneity of coronary heart disease risk factors in Indian, Pakistani, Bangladeshi, and European origin populations: cross sectional study. BMJ. 1999;319(7204):215-220.
10. Dahlen GH. Lipoprotein(a) in cardiovascular disease: Review article and viewpoint. Atherosclerosis. 1994;108:111-126.
11. Low PS, Heng CK, Saha N, Tay JS. Racial variation of cord plasma lipoprotein(a) levels in relation to coronary risk level: a study in three ethnic groups in Singapore. Pediatr Res. 1996;40(5):718-722.
12. Krishnan A, Yadav K, Kaur M, Kumar R. Epidemiology to public health intervention for preventing cardiovascular diseases: the role of translational research. Indian J Med Res. Nov 2010;132(5):643-650.
13. Reddy KS. Rising burden of cardiovascular diseases in India. In: Sethi KK, ed. Coronary Artery Disease in Indians: A Global Perspective. Mumbai: Cardiological Society of India; 1998:63-72.
14. Prabhakaran D, Jeemon P, Goenka S, et al. Impact of a worksite intervention program on cardiovascular risk factors: a demonstration project in an Indian industrial population. J Am Coll Cardiol. May 5 2009;53(18):1718-1728.
15. World Health Organization. CVD-Risk Management Package for low- and medium-resource settings. http://whqlibdoc.who.int/publications/2002/9241545852.pdf
2002. Accessed August 7, 2011.
16. Paradis G, Chiolero A. The cardiovascular and chronic diseases epidemic in low- and middle-income countries a global health challenge. J Am Coll Cardiol. Apr 26 2011;57(17):1775-1777.